Alison Lovkay
Portfolio
2. Understand how to set up and individualize each patient’s exercise program by using past medical history and risk stratification and eventually be able to progress a patient through their program.
Risk Stratification:
Stress Test Findings: There are six different parts of a stress test that help us determine what level of risk a patient is. These findings are ischemic respones on stress test, ischemic response by perfusion imaging, hemo dynamics, functional capacity, ectopy, and angina. Iscehmia is inadequate blood flow to the heart and can be found by looking at the EKG on the stress test or at the wall motion during a stress echo. Hemodynamics would be the response in blood pressure and pulse rate. Functional capacity is how they perform on the test and is measured by looking at their max MET level. Ectopy is shown by looking at the EKG during exercise to see if any unknown arrhythmias occur. Angina is the presense of chest pain.
Non-Stress Test Findings: There are five other factors to look at when determining risk. These are ejection fraction, hospital course, cardiac arrest, congestive heart failure, and depression. Ejection fraction is the amount of blood pumped out by the left ventricle each heart beat. Hospital course looks at what happened while the patient was at the hospital and if there were any complications. Cardiac arrest looks at whether or not the person has been in arrest before and whether or not it was during the event. Congestive heart failure puts the patient more at risk so they look at if they have been diagnosed or if they are having symptoms.
Low Risk:
-
Ischemic Response on GXT: No ischemia
-
Ischemic Response by perfusion imaging: Fixed defect or no reversible defects
-
Hemo dynamics on GXT: Normal
-
Functional Capacity: >7 METS on most recent GXT
-
Ectopy: Absense of complex venctricular arrhythmias at rest
-
Angina: Absense of anginal symptoms with exercise
-
Ejection Fraction: >50%
-
Hospital Course: Uncomplicated MI or revascularization procedure
-
Cardiac Arrest: None
-
Congestive Heart Failure: Absense of CHF
-
Depression: Absense of clinical depression
Moderate Risk:
-
Ischemic Response on GXT: <2 mm of ST segment depression
-
Ischemic Response by perfusion imaging: Small to moderate size reversible defect. Increasing wall motion abnormaliy on stres echo
-
Functional Capacity: <7 METS on most recent GXT
-
Angina: Anginal symptoms controlled by medical management or occuring at <7 METS
-
Ejection Fraction: 40-49%
High Risk:
-
Ischemic Response on GXT: >2 mm of ST segment depression
-
Ischemic Response by perfusion imaging: Large reversible defect
-
Hemo dynamics on GXT: Presence of abnormal hemodynamics
-
Functional Capacity: <5 METS with symptoms
-
Ectopy: Resting complex ventricular dysrhythmias or complex ventricular arrhythmias with exercise
-
Angina: Anginal symptoms at sub-maximal workloads (<5 MET's)
-
Ejection Fraction: <40%
-
Hospital Course: Complicated MI or revascularization procedure
-
Cardiac Arrest: Survival of cardiac arrest within past 6 months
-
Congestive Heart Failure: Presence of CHF < 12 months
-
Depression: Presense of clinical depression
Monitoring:
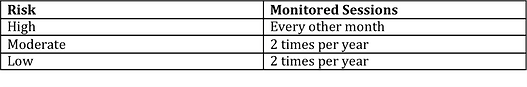
Monitoring telemetry is a very important and useful tool at Cardiac Rehab. Depending on what risk the patient has, the number of monitored sessions changes. This is because a patient who is at high risk is at greater risk for another episode and we want to catch any irregularities that may occur during exercise. We use the telemetry to see if any known ectopy is occuring more frequently, if any new ectopy has started or to see if their normal sinus rhythm has changed. The patient is hooked up to a three lead EKG and monitored on our computers for the duration of that session. Below are the tables that determine how often a patient is monitored. The first is for cardiac rehab, the second for pulmonary rehab and the third is for the maintenance program.
Cardiac Rehab:
Pulmonary Rehab:
Maintenance:


Please visit the page to see the progression of one of my patients